Diary of a Night at Our Central Park Hospital
As night falls in New York City,
a dedicated team of medical professionals show up for work at the Samaritan’s Purse emergency field hospital in Central Park.
This is the story of the night as they battle the deadly COVID-19 pandemic in the tents.
The night shift arrives at the emergency field hospital for their shift. Most of them have gotten just a few hours of sleep despite having gotten back to their rooms 11 hours ago. They’re tired but restless, a mixture of fatigue and adrenaline that keeps them tossing around in their beds. Even as they drive back to the site, they know they never actually left it.

Nurses begin checking in on patients.

"Every night when we come in, we pray that we won’t see the same faces, that our patients from the night before have graduated to step down. It is heartbreaking to see the same people here every night fighting for life. We love them and just want to see them whole and healthy again."
Nurse Anesthetist Corinne
All is peaceful. There are six patients in ICU—four men and two women. They all seem sound asleep. You would never know that they are fighting for their lives. You can hear the sound of the oxygen flowing, like the tent itself is breathing. Nurses check on each patient, stroking their foreheads and holding their hands as they talk to them. There’s no indication that the patient knows what is being said, but the nurses talk anyway, almost as if to reassure themselves that there is still life and connection.
They go about their work meticulously, taking all necessary steps for infectious disease protocol. It is important that they keep themselves safe as well. They have read the reports of healthcare workers getting sick, and yes, even dying. They don’t want to be a statistic, but they aren’t afraid either.

“We’re all just praying for one night when things go smoothly, when patients don’t code. There’s a moment every night as we’re coming in and passing our colleagues who are coming out. And we see the weariness on their faces. And the weight of all of it hits you—how many people have gotten sick, how many have died. But that’s just a minute. Then you take a deep breath and you pray and you walk into the ward and you see these patients that need you and you get to work.”
Nurse Brendan
The silence is shattered as a patient is rushed into ICU. He is thrashing, gasping for air. The nurses shout his name and try to comfort him, to calm him. If only he could understand that they’re there to help. But he is fighting this team, who is desperately trying to get him the oxygen he needs. Beads of sweat pool at the line where his forehead meets his curly gray hair. After five minutes of struggle—five minutes that feel like an eternity—he is finally at peace. He has breath again, even though it is breath that goes in and out of his lungs at a frantic pace. The team is then able to get to work. Large tubes go in. Small tubes go in. By 8:22 PM, all is quiet again. The patient’s family calls. The doctor assures them that he’s stable. He’s now on a ventilator. He’ll get good care here. This family is calm. The doctor says not all of them are.
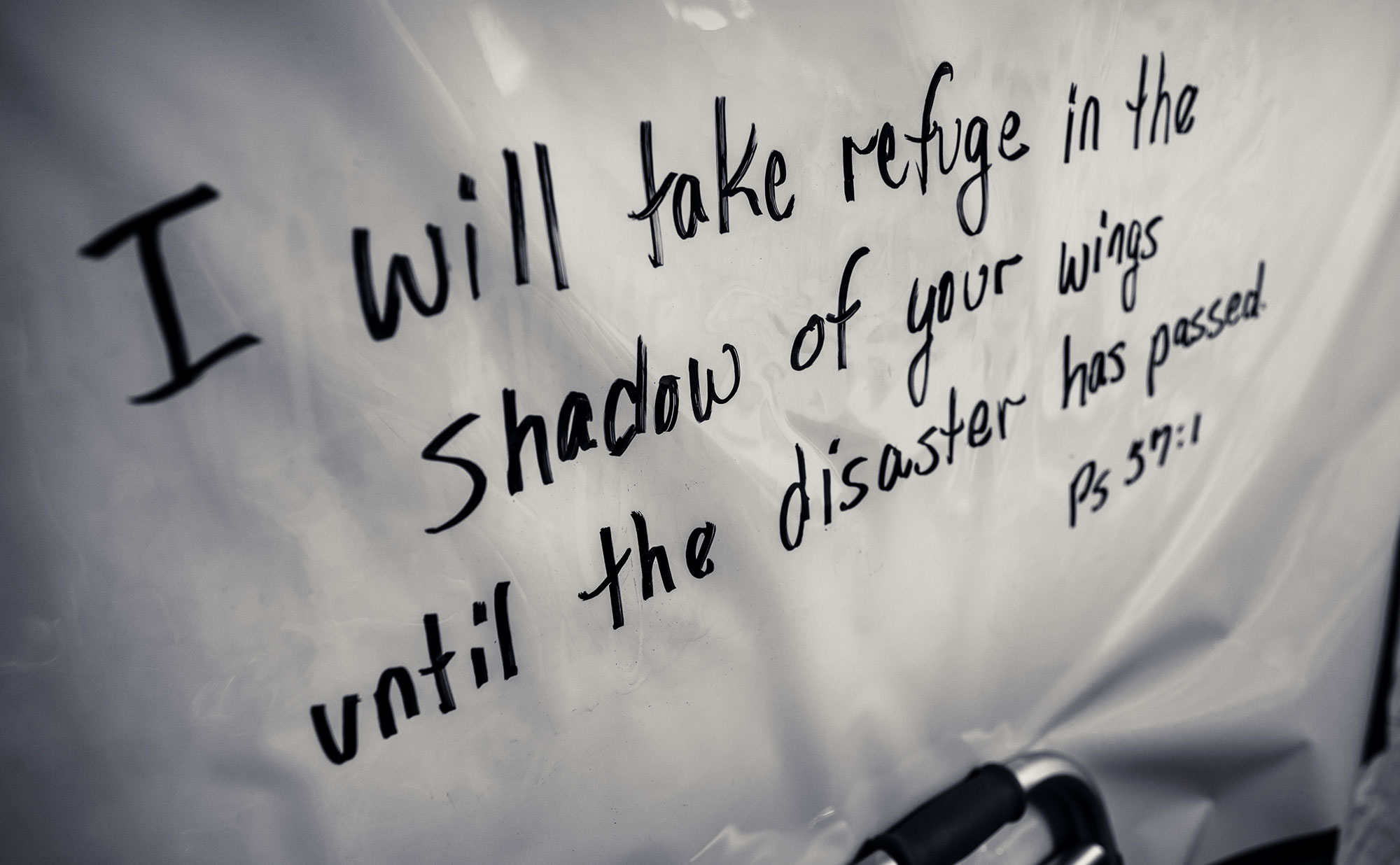
A patient wakes up. He’s a man in his 50s. The nurses remove his bedpan and tenderly clean him. He looks embarrassed to be reduced to having someone wipe him clean. They cover him with a new, clean warm blanket, and their eyes smile at him through the plastic protective shield. When they turn him sideways, he is able to help them. They call him “strongman,” and the corners of his mouth try to force themselves into a smile around his breathing tube. His wife has told them that he is stubborn, but that he has a strong faith. She asked if the staff would pray for him and their family. They ask him if it would be OK for them to pray for him at this moment. He nods yes and shuts his eyes again. Later, they say he tries to exert himself too much, and they have had to change his tubes frequently because of the secretions that harden inside of it. They become like rocks blocking the airflow in the tube. It’s like breathing through a coffee stirrer instead of a straw.
There’s camaraderie here. These people have known each other for less than two weeks, and now they have to function as a team. But they’re more than a team, they’re like blood. They know how to work with and around each other. There’s no bickering, no petty complaints. There’s no time for the things that don’t matter. Here and there, they are able to spend a minute or two talking to each other about their hometowns, their families. Sometimes, that’s the only way to cope.

The strongman crashes. His oxygen saturation drops suddenly and his pulse fades. A team of five rush to his bed. Once again, his breathing tube is clogged by secretions that look like rocks. One of the team hooks up what looks like a plastic two-liter bottle and begins squeezing to breathe for him. They work frantically—turn off the propofol, we need atropine now, please help us Heavenly Father. They are able to get his oxygen saturation back up to 96 percent and can feel his femoral pulse come back strong again. They get his tubes changed. The physical effort of saving his life in that moment would have exhausted anyone. They should rightfully be able to sit down and gather their own breath and thoughts. But there’s no time for that. At 10:07 PM, they thank God for His mercy in saving this patient and thank each other for the teamwork before moving on to care for the other patients.

A woman in her late 50s is sitting up in bed trying to cough up mucus. Three nurses are gathered around her, encouraging her to get it out. She is struggling; nothing will come. She says that it is hopeless. She is worried that she will get worse. She knows how this could end. She apologizes to the nurses for being so much trouble. Nurse Karman says, “That’s why we’re here, to care for you. We love you.” Nurse Erin rubs her arm with double-gloved hands. She has to wear them to protect herself, but compassion moves through any barrier. The nurses begin patting her back, and finally a large wad of mucus comes out. The nurses encourage her and show her that her oxygen saturation level is rising. She and her family have expressed that she is a person with strong Christian faith when she arrived at the hospital. The nurses ask her if she would like for them to pray for her, and she says, “Yes, I would like that very much. Please.” Nurse Erin begins to softly hum hymns. The patient keeps her eyes closed and leans into the sound. Her oxygen level continues to rise. They ask her if she wants to lie back down. She says that she feels good now and would like to continue sitting up. She has hope again.
One of the patients begins to wake up and tugs at her ventilator tube. She doesn’t speak English. A Spanish-speaking nurse rushes over to calm her. She explains that even though the tube is uncomfortable, it is necessary. What she doesn’t say is that the tube is the only thing keeping her alive. She doesn’t want to scare her. She rubs her head, and the patient begins to calm down. She asks the patient if she would like to listen to some Spanish music, and the patient nods yes. The nurse pulls up her favorite playlist on her phone and lays it on the patient’s shoulder near her ear. The patient’s face softens, and she stops struggling. The nurse asks if she likes the music, and she nods yes.

The medical professionals are reluctant to take breaks, to leave their patients, but they know it’s a must for their own physical and emotional health. Because of infectious disease protocols, there is no eating or drinking in the wards, and the Personal Protective Equipment (PPE) gets hot, even when the temperatures outside the tent hover in the low 30s. They send each other out—one or two per ward at a time. Nurse Kirsten decides she can finally pull herself away for a few minutes. The first step is taking off the layers of protective gear that has kept a barrier between her and the virus as she touches her patients to provide care. Removing each layer is liberating, but she is doing it in the cold night air. And with each layer, she has to wash her hands in chlorinated water, which is also freezing cold. When the last piece is off, she rushes to the food tent and loads up on cold Mac and cheese, Diet Coke, and a slab of cake that was donated from a local bakery earlier in the day. She settles into a blue plastic Adirondack chair in the eating tent and digs in. There are already about a half dozen others in the warm tent trying not to fall asleep as the heated air blows through. At first, they try to avoid talking about the virus that has consumed their life, but the conversation inevitably turns back to the disease they call “the night monster.”

“I’ve been caring for patients for 40 years, and I have never seen so many people gasping for air at the same time. I’ve just never seen anything like it. People who were living their normal lives this time last week are now fighting for each breath. It’s like an alien landed on earth and started pulling people off of the sidewalks and sentencing them to death.”
Nurse Practitioner Tim

“It’s like at midnight each night, you can see the cytokine storms erupt. They all spike fevers at the same time, and their bodies become chaos. All of them. All at the same time. Every night. This isn’t the flu. This is nothing like the flu.”
Nurse Anesthetist Kirsten
They all agree that Joanne is the true hero. She’s a staff member that serves as a runner to make sure they are fully stocked with the medications and other supplies that will keep their patients calm and breathing. When the group’s attention moves to her, she giggles and shrugs. Then a request from the ward comes over the radio, and she hustles out of the tent to get more supplies to the wards.
At the end of the break, it’s time to don the PPE again. Two pairs of gloves, coveralls, N95 mask, hair cover, rubber boots, and face shield. It’s a long process and each one checks the other to make sure no step is overlooked. Despite this, they go as quickly as they can so that others can get a break too.

Almost all of the beds are full with men in their 50s, except one where a man in his late 80s is resting peacefully. Nurse Sonja watches over her sleeping patients, keeping a particularly close eye on him. She says their status can change so suddenly it’s like whiplash. Fortunately, she thinks a few might be able to go home tomorrow, but it makes her sad that the night shift never gets to see them walk out, to celebrate their victory with them. "I wish we could get our chance to cheer too."
Nurse Sonja works the day shift at home in Cheyenne, Wyoming. At first, she wasn’t thrilled about being assigned to nights. But now she appreciates the time she gets with her sleeping patients. “There’s something about the night shift that has made me feel more deliberate in the way I care for them. I can’t explain it. There’s just something about the night.”

"I thought they would be freaked out by being in a tent hospital. It isn’t what anyone in America would ever dream of. But I think they’re all just so thankful to be here, to get this care. They know they’re safe here, and it just doesn’t even matter that they’re in a tent anymore."
At 3:20 AM, the announcement comes over the radio. The patient in Bed 20 has passed away. Sonja looks down at her feet and sighs. “That wasn’t my patient, but it hits us all hard when we lose one. We didn’t come here to lose them.”
Nurses Chelsea, Ann, and Tim continue to prepare the body of the patient in Bed 20 to be taken to a morgue off-site. This isn’t the first patient they have lost, and they each know their places as they perform this last act of service for this man. They tenderly clean him and then fill out the paperwork—a stack of white sheets with facts and signatures that are the final confirmation that a life has ended. They gently place the body in a white bag and seal it then transfer it to a gurney to be wheeled out of the tent. It takes the strength of all three of them to lift him. The patient in Bed 21 is resting peacefully, unaware of what has taken place next to him. Of all the patients in the ward, he is the most stable. An elderly man across the aisle who has requested not to be resuscitated struggles with the mask that covers his face and pumps oxygen into him. Next to him are two others who are on the edge of being transferred to the ICU. One of them is a man in his 50s, dark hair, arms covered in tattoos. Nurse Chelsea said last night he had moments of coherence.
"He said that he knows we’re different here. He can see that there’s something different. I could tell he was reaching out for comfort, so I told him a children’s story. My mom is a big fan of children’s books, and for some reason I just fell into that like she does. It’s funny how you fall into those things without even thinking, but he liked it."

The strongman is awake again. He has no idea how severe his situation was just a few hours ago. The nurse tells him he’s looking good, and he waves his big hand at her, then a thumbs up. He wants to sit up, to communicate. They tell him not to exert himself too much. His head falls back again, eyes close, and his chest rises and falls in a steady rhythm. Everyone is asleep again with the pulsing sound of the oxygen swirling around them.
The final and hardest two hours of the shift have begun. They do their rounds once more, taking specimens for labs and checking vitals. They want to finish strong—no more crashes, no more deaths. They want to hand off peaceful wards to their day shift counterparts. Their eyes plead with each patient—keep fighting, and we promise we will too.

The teams begin boarding the shuttle back to their rooms. They have shed most of their PPE, but their masks are still on. They can’t even look into the full faces of their brothers and sisters in the battle. The shuttle is silent. The quiet is cut by a reminder that comes with the sunrise. There’s a verse in the Psalms that says, “Weeping may tarry for the night, but joy comes with the morning.”
“Weeping may tarry for the night, but joy comes with the morning.”
Psalm 30:5 (ESV)

Emergency Medicine
Whether sending an Emergency Field Hospital to Italy or New York City in the wake of COVID-19, setting up treatment centers in the midst of an Ebola outbreak, or offering care in the midst of armed conflict, Samaritan's Purse stands ready to respond in the face of a myriad of medical crises. Your gift will help bring expert treatment and the hope of the Gospel to the sick and suffering.




