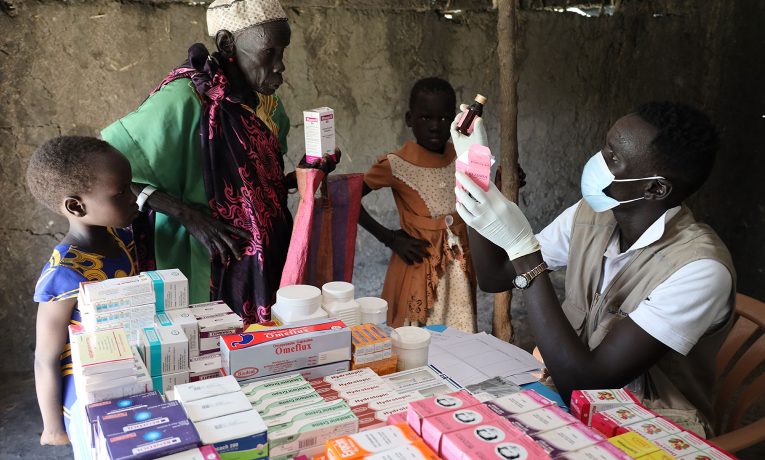
Samaritan’s Purse Mobile Medical Units are bringing critically needed healthcare to remote villages.
Nyawika, her mother, recounted the day three years ago when it all started. Kawine was busy about the afternoon’s duties, and the other children were playing in the shade of a tree. Then suddenly Nyawika “heard the siblings crying for help so I ran to them,” and she found Kawine shaking on the ground.

Kawine received severe burns from falling in a cooking fire during a seizure.
Everyone hoped it had only been a malarial fever causing the convulsions. The seizures continued, though, despite malaria pills from a local pharmacy.
Night and day Nyawika tried to watch Kawine to ensure she didn’t hit the ground or brush against the cooking stove or fall into the fire. Tell-tale bruises and burns showed there weren’t enough eyes to protect the girl as the episodes struck without warning.
This Is Not a Bewitching
The mother and her ailing daughter spent most of two years in another town seeking help from a spiritual healer. Nyawika had been convinced by family and friends that what afflicted Kawine was the work of a curse.

Some of our mobile medical teams navigate flooded areas in dugout canoes.
“The spiritual healer was demanding a lot of money from us for the traditional healing,” Nyawika said, remembering how the man’s traditional practices seemed only to agitate the situation.
Then the Samaritan’s Purse mobile medical unit (MMU) arrived in their home village of Koatna Ruathnyibol Payam. Hearing good news from a relative about our work, Nyawika and Kawine came to see our team. In fact, Kawine had been burned just the night before after falling into a cooking fire while seizing. It was the worst burn she had suffered of the previous three years.
When she walked into the MMU with her mother, the medical team began dressing her wounds, offering prayer and encouragement for the two, and delving into the symptoms that brought them there.
It wasn’t long before they had some answers to their issues. At the words of the doctor, relief began to wash over Nyawika.
“Your daughter is not bewitched,” one of the doctors explained. “We don’t understand all that has caused her illness, but she has something called epilepsy. And there are medications for this condition.”
Nyawika and Kawine left the MMU that day with medicine and with the hope that this was the end of their long road of treatment. Only the coming months would tell.
Beginning Anew Back Home
We praise God that it’s now been several months since her treatment began and as many months since her last seizure. Each month Nyawika returns for the medication and to bring a report, and the reports have been good.

The medical team also provides training for disease prevention.
“I am forever grateful for the medical team for their exemplary help,” she said. “I’m not incurring the expenses for Kawine’s treatment anymore, and now her health has improved.”
For people like Nyawika and Kawine, living in remote places like Koatna Ruathnyibol Payam, basic medical care would be virtually out of reach. At the very least it would require travel across long distances, often on foot, often for hours, to healthcare facilities that are ill-equipped and understaffed.
Our Mobile Medical Units are traveling long distances in these remote areas of South Sudan to provide emergency and primary care, education in the prevention of communicable diseases, and emotional support through trained clinicians.
In most cases, the MMUs are providing care in communities where our other programs have been established, including agriculture and livelihoods; water, sanitation, and hygiene (WASH). Each unit has the capacity for seeing up to 200 patients per day.
All this in a region where maternal mortality and neonatal deaths are on the rise, where malnutrition is an ongoing threat, where mass flooding has stifled growing seasons, and where families can spend years of their lives chasing down treatments that don’t work.
For Nyawika’s family, their journey has ended in joy. They’ve been able to set up their home again and re-established their lives after those lost years.
“This year I am able to cultivate my garden and provide basic needs,” Nyawika said. “Such as food for my children.”

Our mobile medical units operating in South Sudan are providing a variety of care to remote areas of the country.